Educating the healthcare workforce of the future: lessons learned from the development and implementation of a ‘Wearables in Healthcare’ course

Abstract
Digital health technologies will play an ever-increasing role in the future of healthcare. It is crucial that the people who will help make that transformation possible have the evidence-based and hands-on training necessary to address the many challenges ahead. To better prepare the future health workforce with the knowledge necessary to support the re-engineering of healthcare in an equitable, person-centric manner, we developed an experiential learning course—Wearables in Healthcare—for advanced undergraduate and graduate university students. Here we describe the components of that course and the lessons learned to help guide others interested in developing similar courses.npj Digital Medicine (2023)6:214 ; https://doi.org/10.1038/s41746-023-00964-y
Introduction
Healthcare lags far behind virtually every other industry when it comes to taking advantage of digital technologies. Despite that current reality, there is near uniform recognition by major global and national health organizations that digital technologies will shape the future of healthcare. Framing the full scope of the necessity and the challenge of making that a reality, the WHO states, “Digital health should be an integral part of health priorities and benefit people in a way that is ethical, safe, secure, reliable, equitable and sustainable”. Wearable sensors can be a key component of a digital transformation of healthcare globally. While most of the physiologic measures that wearables track (e.g., heart rate, respiratory rate, and temperature) are not dissimilar from what is currently measured in healthcare, the wearable-derived versions are uniquely different enough to transform them into individualized vital signs. For example, while a person’s heart rate may be measured over a 10–30 s period every few months or years in the medical office setting, wearables provide near-continuous heart rate data, including routine variation during specific types and levels of activity. These kinds of data allow for the establishment of a “healthy baseline” and the detection of unexpected deviations from that baseline, creating a dynamic, vital sign for each individual. Extracting actionable information from these large, multivariable, and longitudinal data streams comes with substantial challenges. For one, the data are orders of magnitude messier than the well-controlled snapshot of vital signs obtained in the healthcare setting. Separating out the signal from the noise requires data analytic expertise as well as an understanding of the potential health impact of trade-offs between accuracy, latency, and volume.
An understanding of how the use of wearable data can impact individuals and communities is critical to understanding their potential role in healthcare. For example, since wearable data can lead to health concerns and create anxiety, 24/7 bidirectional, individualized communications capabilities are required to address this in a person-centric manner. In addition, appreciating how wearables can further exacerbate—rather than help eliminate—existing health disparities if not thoughtfully implemented is especially important. Assuring that wearables’ role in the future of care drives health equity requires knowledge of existing gaps, historical biases, and purposeful, equitable solution design. In order to better prepare the future health workforce with the knowledge necessary to support the re-engineering of healthcare in an equitable, person-centric manner, we developed an experiential learning course—Wearables in Healthcare—for advanced undergraduate and graduate university students. Here we report the structure, experience, outcomes, and learnings from this course so that other educators can potentially build off our experience and develop similar courses that will help further accelerate the transformation of healthcare.
Course description
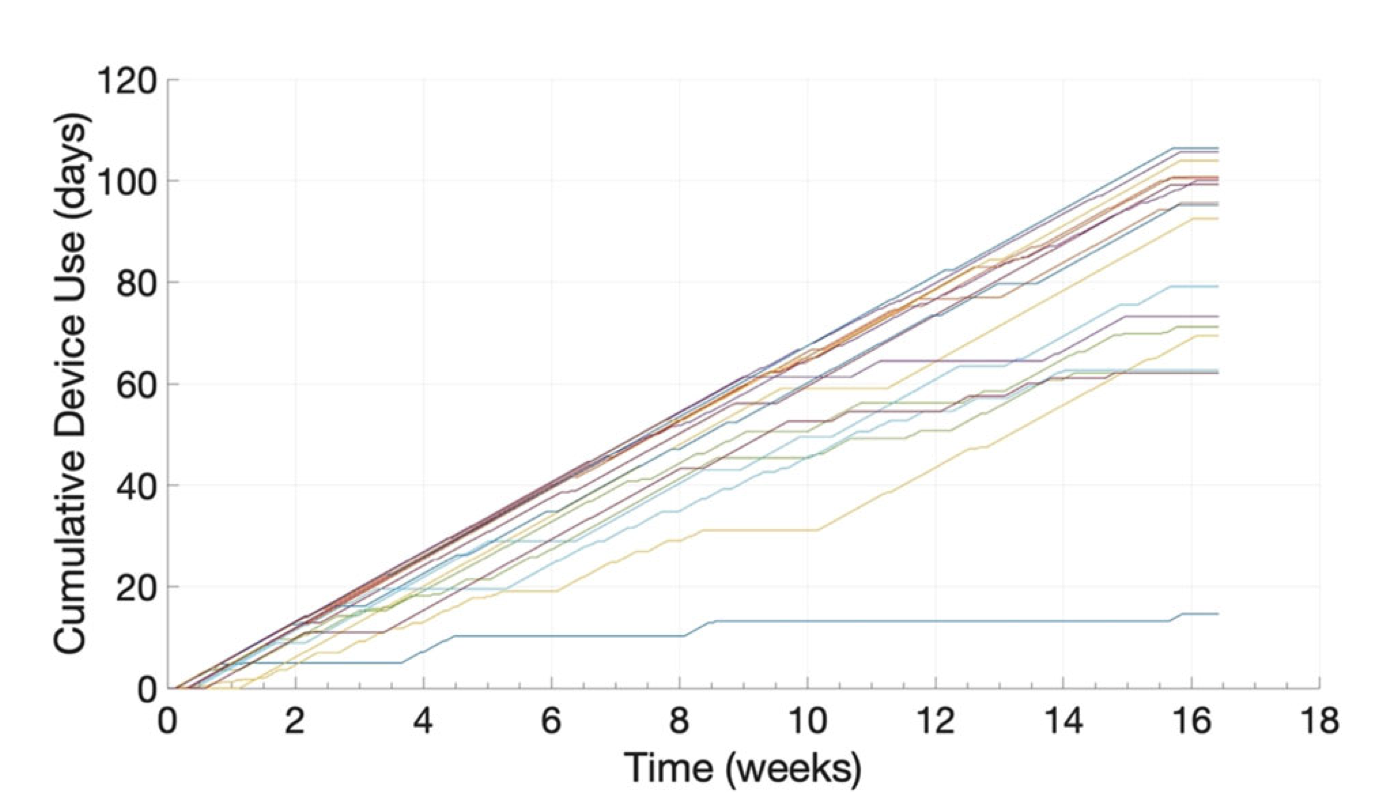
The Wearables in Healthcare course was developed, in part, to directly expose students to the challenges and opportunities surrounding the use of wearable data in healthcare, the origin and meaning of physiologic signal dynamics measured or derived from data collected by wearable sensors, and the skills needed to process and interpret these continuous data streams. To facilitate a hands-on, real-world experience, all students were given a medical-grade wrist sensor to wear throughout the semester, along with access to all of their raw data streams to permit analysis of their own data. This pairing of personal wearable sensors and data, along with directed reading, lectures, and labs, provided students the opportunity to learn first-hand about their unique physiologic responses to routine behaviors and the difficulties in extracting that information in the most meaningful way. Throughout the 16-week semester, the class exposed them to the multiple challenges that need to be overcome to make these technologies more pervasive in healthcare.

Fig. 1 The Corsano 287-2B. Sensors and metrics available from the medical-grade wearable used by students