Introduction
Atrial arrhythmias, notably atrial fibrillation (AF), constitute a paramount concern in geriatric health, serving as a precursor for an array of complications such as stroke, heart failure, and enhanced mortality rates. Contemporary methodologies for detecting atrial arrhythmias, albeit efficacious, occasionally falter in terms of timeliness, continuous monitoring, and patient compliance.
Background
Atrial fibrillation (AF), the predominant cardiac arrhythmia, currently affects approximately 37.574 million individuals worldwide, equivalent to 0.51% of the global population. In 2017 alone, there was a documented addition of 3.046 million new AF cases, reflecting an incidence rate 31% higher than that recorded in 1997. While nations with a high socio-demographic index bear a significant AF burden, the steepest increases have been observed in countries with a middle sociodemographic index.1 The repercussions of undetected or tardily diagnosed atrial arrhythmias are profound. These irregular heart rhythms, when left unchecked, augment the risk of cerebrovascular accidents or strokes, accounting for nearly one-third of all stroke-related hospitalizations in the elderly cohort. Moreover, untreated AF precipitates a five-fold surge in stroke risk, exacerbates the potential for heart failure, and can culminate in diminished quality of life owing to palpitations, fatigue, and dyspnea.2 Presently, standard practices for AF detection encompass electrocardiograms (ECGs), Holter monitors, and event recorders. While
these modalities have demonstrated efficacy, they are not devoid of limitations. ECGs provide only a fleeting snapshot of cardiac activity and may not capture sporadic arrhythmic events. Holter monitors, despite their capability for extended monitoring, are constrained by their typical 24- to 48-hour recording window. Event recorders, though enabling longer durations of monitoring, are contingent on the patient's proactive involvement to record perceived irregularities. Additionally, the lack of real-time data transmission in many conventional devices renders timely interventions challenging. This diagnostic lacuna necessitates an exploration into innovative, technologically sophisticated alternatives capable of revolutionizing the landscape of atrial arrhythmia detection.
1 Lippi G, Sanchis-Gomar F, Cervellin G. Global epidemiology of atrial fibrillation: An increasing epidemic and public health challenge [published correction appears in Int J Stroke. 2020 Jan 28: 1747493020905964]. Int J Stroke. 2021;16(2):217-221.
2 Sanders GD, Lowenstern A, Borre E, et al. Stroke Prevention in Patients With Atrial Fibrillation: A Systematic Review Update. Rockville (MD): Agency for Healthcare Research and Quality (US); October 2018.
Findings from a landmark study
The exploration into innovative atrial arrhythmia detection methodologies led to the initiation of the "Smartphone and Wearable Detected Atrial Arrhythmia in Older Adults Case Finding Study" (Smart in OAC—AFNET 9). This study combined modern consumer electronics with rigorous scientific analysis to assess the feasibility and efficacy of these tools within an older population.3Methodology
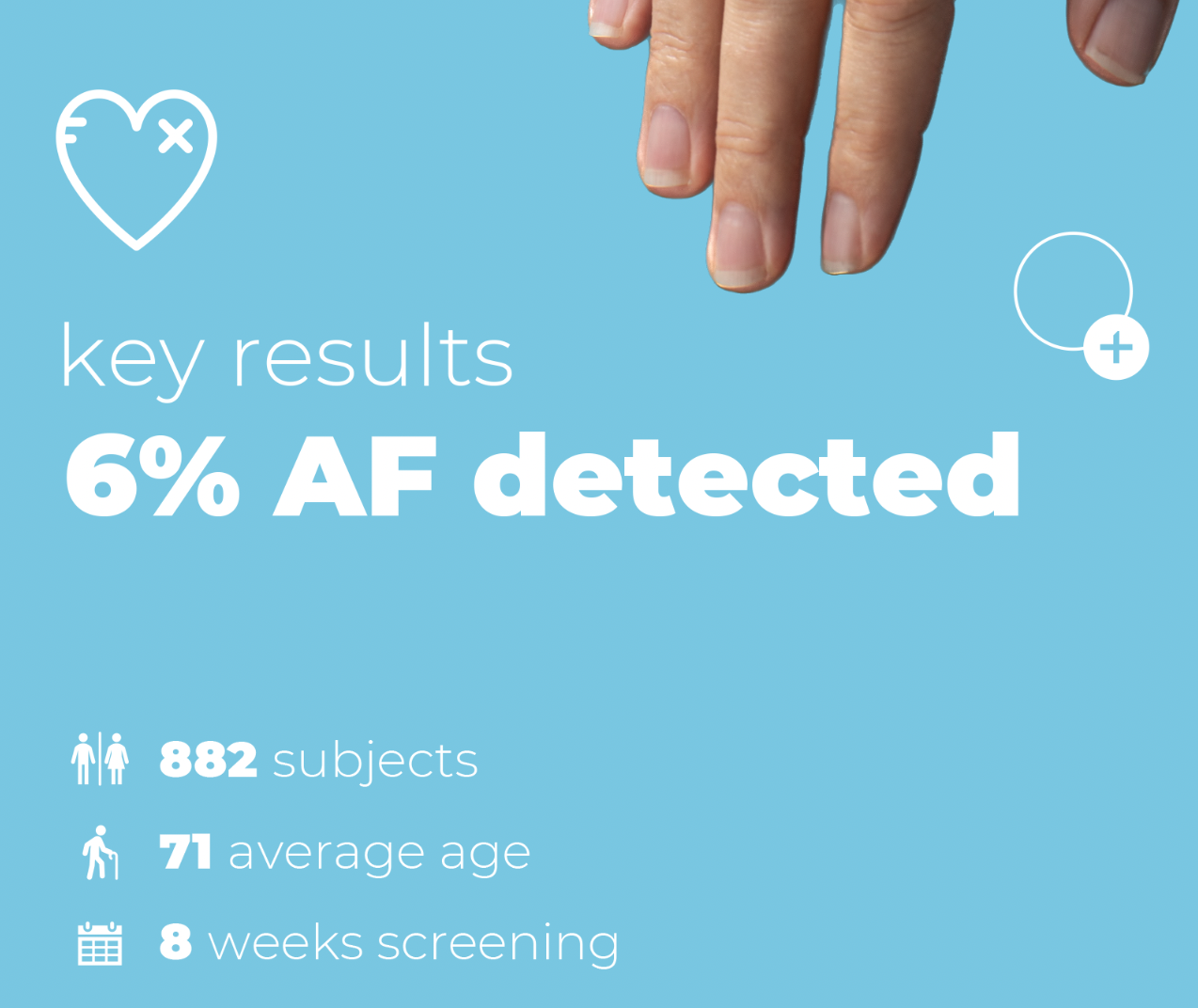
The study involved 882 individuals aged 65 and older from Germany, Poland, and Spain, a demographic traditionally at higher risk for atrial arrhythmias. These participants, who had no known history of atrial fibrillation and were not undergoing anticoagulation therapy, were enrolled digitally for an 8-week, fully remote study utilizing innovative data collection techniques. The enrollment leveraged media communications and direct contacts, with 53% of participants completing all procedures remotely, highlighting the growing trend toward digital health solutions.
Central to this study's data collection methodology was the use of the Corsano CardioWatch, a medically certified wearable with a photoplethysmography sensor. This device interfaces directly with smartphones, enabling detailed cardiac data acquisition. It continuously monitors up to 19 vital parameters, including pulse rate, heart rate variability, ECG, and SpO2. With an integrated real-time research platform, the CardioWatch facilitates direct access to raw data, suitable for artificial intelligence (AI) and machine learning (ML) analysis.
3 Fabritz L, Connolly DL, Czarnecki E, et al. Smartphone and wearable detected atrial arrhythmias in Older Adults: Results of a fully digital European Case finding study. Eur Heart J Digit Health. 2022;3(4):610-625. Published 2022 Nov 1.
Results
The cohort comprised a total of 882 individuals, with an age distribution of 71 ± 5 years, ranging between 65 and 90 years. Out of these, 500 participants (57%) were female. Concerning health profiles, 414 participants (47%) reported a history of hypertension, and 97 (11%) indicated a diagnosis of diabetes.

Extending the monitoring timeframe to the full 8 weeks led to the detection of arrhythmias in 53 participants (6%).
Leveraging the Corsano CardioWatch offered a nuanced insight into the data. The device's capability to monitor various vital parameters provided a comprehensive profile of each participant's cardiac health, while the real-time transmission and storage of data on the secure health cloud facilitated instant access to results and trends. The CardioWatch's AI and ML compatibility enhanced the data's depth, providing refined analysis and potentially shedding light on preliminary markers or trends preceding the onset of arrhythmias. A direct comparative efficacy analysis between traditional methods and the CardioWatch remains a potential avenue for subsequent research.